Introduction
For lipophilic drug substances that exhibit dissolution-rate limited absorption (BCS II and IV) self-emulsifying drug delivery systems (SEDDS), which are defined as “isotropic mixtures of oils, surfactants, solvents and co-solvents”, are a viable approach to enhance bioavailability.
SEDDS are relatively simple formulations to develop; the simplest systems comprise an oily vehicle (lipid), a surfactant, and a co-surfactant and optionally, and an antioxidant. Alternatively, a single excipient with self-emulsifying properties can be used.
Preparation of SEDDS simply involves adding all the hydrophobic ingredients together and heating to 50 oC. In a separate container the aqueous phase (solvents and surfactants) is also heated to 50 oC. The two phases are then blended to form SEDDS. This is illustrated below:
Figure 1: Preparation of a simple SEDDS Formulation
The system is designed to form a fine and stable oil-in-water (o/w) emulsion upon contact with digestive fluids and the agitation from the digestive processes. SEDDS can be dosed into either softgels or two-piece hard capsule shells.
A key aspect of SEDDS is the use of digestible lipids. These are required not only to carry the drug substance but also to provide the desired pharmacokinetics while minimizing food effects and variability.
The improvement in oral absorption for SEDDS, which depends on many formulation-related parameters, such as surfactant concentration, oil/surfactant ratio, polarity of the emulsion, droplet size and charge, all of which in essence determine the self-emulsification ability, is due to increased intestinal absorption via supersaturation, tight junction modulation, and reduced first-pass effect.
Advantages of SEDDS
- SEDDS can be used with both hydrophobic and hydrophilic drug substances, as well as with liquids and solid dosage forms.
- Lower levels of drug used in SEDDS compared with conventional formulations means less incidences of side-effects to consumers.
- Finely divided oil droplets are more uniformly and consistently distributed within the GI tract which enhances absorption and bioavailability, while minimising localised pooling.
- Ease of manufacture and scale- up compared with other drug delivery systems such as solid dispersions, liposome and nanoparticles.
Disadvantages of SEDDS
- Generally, there is a lack of good predicative in vitro models for assessing SEDDS formulations. Traditional dissolution methods are not suitable since SEDDS require in-situ emulsification and digestion prior to releasing the drug.
- The high surfactant concentrations in SEDDS formulations (approx. 30-70%) can instigate chemical instabilities of drug substance or even irritate the GI tract.
- Volatile co-solvents in the SMEDDS formulations are known to migrate into the shells of soft or hard gelatin capsules, resulting in the precipitation of the lipophilic drugs.
- Formulations containing several components become more challenging to validate.
SEDDS Raw Material Selection
Note that there are only a select number of drug substances and excipients or excipient combinations that can efficiently form SEDDS systems.
Drug substance
SEDDS are ideally used to increase solubility of poorly soluble drugs; typically BCS class II and class IV drugs. The drug substance ought to possess enough lipophilicity and affinity to the oily vehicle (log P >2, ideally ³5, and solubility 50 mg/g) to enhance absorption and circulation into the lymphatic system.
Excipients
SEDDS places specific constraints on excipients. Furthermore, the self-emulsification process is specific to the levels and type of the oils – surfactants combination, surfactant – co-surfactant ratios and the temperature at which self-emulsification occurs.
Generally, the following are the materials for consideration:
- Oils: The first choice oils for SEDDS are medium chain triglycerides (MCT) and hydrolysed vegetable oils. These serve as the oily phase and to solubilise the drug substance. The presence of long- chain fatty acids such as oleate and linoleate can help boost the lymphatic absorption of highly lipophilic drug substances, especially if they have logP values of 5 or higher. This tactic can be used to avoid the first-pass
- Surfactants: Surfactant choice is limited to non-ionic surfactants with a high HLB and low oral toxicity. Examples of suitable surfactants include Polysorbate (e.g Span 80, Tween 80) and Hydrogenated castor oil derivatives (Kolliphor RH40).
- Co-surfactants: To lower potential GI tract effects associated with high levels of surfactants needed for SEDDS formulations co-surfactants are added. Co surfactants help lower the interfacial tension to a very low levels that facilitates ‘spontaneous’ emulsification. Examples of co-solvents include polyethylene glycol and ….
- Solvents and dispersants: Solvents and dispersants suitable for oral administration include ethanol, propylene glycol (PG), polyethylene glycol (PEG) and glycerin. Their purpose is to help solubilise the drug substance and surfactant or the drug into the lipids.
Optional excipients
Antioxidant Agents: Lipophilic antioxidants (e.g. α tocopherol, propyl gallate or ascorbic palmitate) to prevent oxidation of oils in SEDDS formulations.
- Viscosity Enhancers: Emulsion viscosity can be improved with the use of additional material such as gums and waxes (glyceryl monostearate, glyceryl tristearate, beeswax and stearic acid).
- Polymers: Polymer may be added at levels ranging from 5 to 10% w/w to form a matrix. Examples of suitable polymers include HPMC, HPC and Ethylcellulose.
- Mesoporous silica: Mesoporous silica can be used to added to convert liquid SEDDS into free-flowing powders that can be filled onto conventional capsule machines or compressed into tablets.
Starting Formula
Material |
Level (% w/w) |
Supplier |
OilsMedium chain triglyceridesGlyceryl monocaprylocaprate |
40 (range 20 – 70)7.5 (range 5 – 15) |
IOI Oleo, BASF, Croda & Gattefosse’ & Abitec |
Primary SurfactantHydrogenated castor oil derivativesPolysorbate 80 |
42.5 (range 30 -70) |
BASF, Croda and others |
Supplementary OilsOlive oilCastor oilOleic acid |
10 (range 10 – 30) |
Pharmacentral |
Co-SurfactantsSorbitan Monooleate Glyceryl Oleate PEG-8 Caprylic/capric glycerides |
10 (range 10 – 20) |
IOI Oleo, BASF, Croda & Gattefosse’ & Abitec |
Co-Solvent(s)Polyethylene Glycol 400Propylene Glycol |
5 (1 – 10) |
Dow Chemical & Sasol |
Anti-oxidantα tocopherol, propyl gallate or ascorbic palmitate |
0.05 |
Merck |
Aqueous PhaseWaterWater/Ethanol |
10 |
– |
Steps for Developing Successful SEDDS formulations
Successful formulation and development of SEDDS requires characterization and optimization of the formulation on the same basis as any other formulations, particularly in respect to drug solubility and loading, dispersibility and stability, and for scale-up studies, to achieve similar performance at larger manufacturing scale as was observed during development stages.
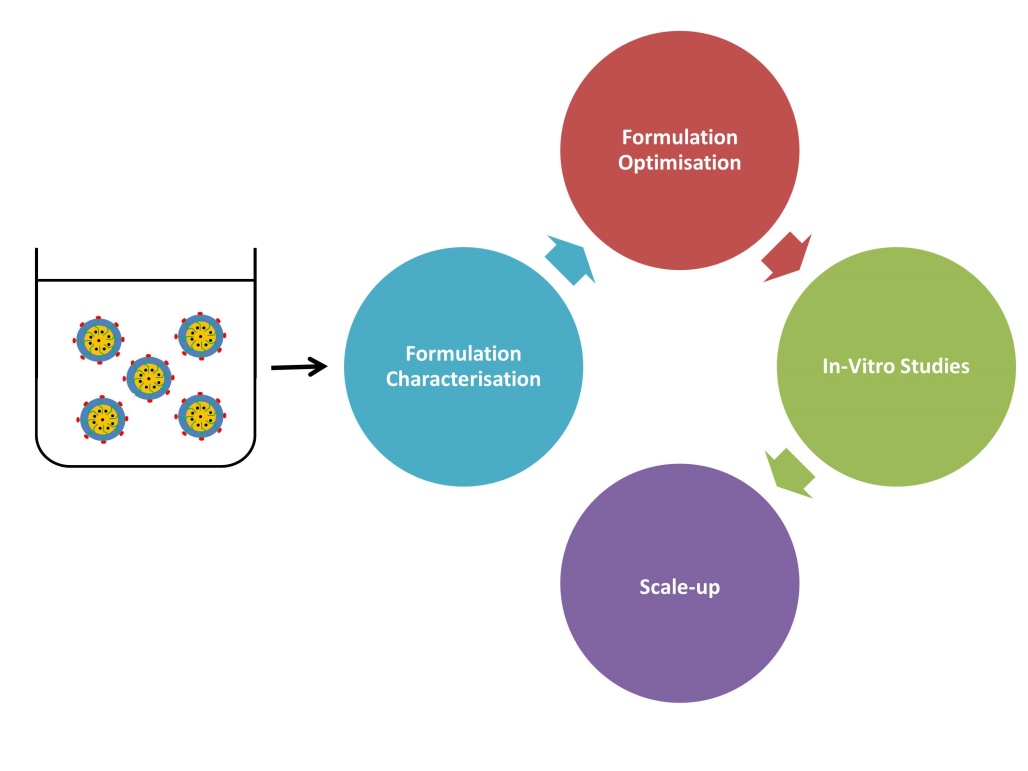 Figure 2: SEDDS Formulation Characterisation and Optimisation
Figure 2: SEDDS Formulation Characterisation and Optimisation
Here below are a number of important ‘must dos’ for optimizing SEDDS formulations:
1. Determine equilibrium solubility at ambient conditions
The first step when developing a SEDDS formulation is to screen the solubility of the drug substance. Solubility is important since it gives the formulator an idea about the formulation’s expected maximum drug loading, stability and performance.
In this respect, equilibrium solubility should be determined at ambient conditions in a range of oily vehicles, surfactants and co-surfactants, as well as their combinations.
Equilibrium solubility in liquid vehicles is determined by equilibrating the drug substance at room temperature and assaying the amount dissolved using HPLC. In solid lipids, equilibration is best achieved at higher temperatures and allowing the mixture to solidify (e.g after 24 hrs) before it is examined by DSC or other suitable technique to establish the saturation concentration.
Frequently prevailing conditions, either from the substance or the dissolution medium, result into the formation of a supersaturated solution, where the amount of solute exceeds the equilibrium solubility. Such supersaturated solutions are thermodynamically unstable, and any such concentration values, represent kinetic solubility values rather than an equilibrium solubility values.
It is therefore important for formulators to make a distinction between equilibrium and kinetic solubility, and to know when a particular measurement represents an equilibrium solubility value, or if the determined value simply represents some type of metastable condition.
Solubility screening should be performed in a wide range of excipients, including solid and waxes. Depending on the type of drug substance, some solid excipients can adequately dissolve and enhance bioavailability. For solid vehicles that become molten at or above their melting points (40°-65°C) before adding the drug substance, the effect of the short heating and cooling rate on the API-formulation stability should be investigated.
When making decisions about the dose of the drug, it is important to limit the drug loading to below 80% of the saturation concentration to prevent nearing the drug’s saturation point in the system. This is because supersaturation can easily put at risk a formulation’s physical stability and potentially lead to crystallization during the product’s shelf life.
- Perform Drug substance and Excipient Compatibility studies
Just like any other formulation project, drug substance – excipient compatibility studies constitute an important aspect of a SEDDS formulation programme. These studies serve to identify, quantify and predict any unwanted interactions (chemical and physical) as well as their significance on quality and performance of the product. The end game is to arrive at excipients that will be incorporated into the formulation. DSC and stress studies of binary and ternary blends can be performed by stressing blends and any degradants assayed using HPLC, IR or mass spectrometry.
3. Evaluate the Formulation’s Dispersibility
Dispersibility of a SEDDS formulation is undertaken to determine its capability to disperse into a fine and stable emulsion. The test relies on measuring the size of resulting emulsion dispersed phase and is undertaken using a standard USP Type 2 dissolution apparatus (Paddle Type).
One ml of each formulation is added to 500 ml of water at 37 + 0.5ºC and the paddle is rotated at 50 rpm. The SEDDS formulation should form a mixture or gel which is of different type depending upon which the in vitro performance of formulation. Nano or micro – emulsions, which are desired for SEDDS, form rapidly to yield a clear, bluish or slightly less clear emulsion, having a bluish-white appearance.
In addition to in-vitro dissolution tests, it is necessary to test the formulation under lipolysis conditions. This is because lipid digestion in the gut is the main physiological event that enhances the bioavailability of poorly soluble compounds. As the SEDDS formulation disperses and emulsifies in the GI tract, lipolytic enzymes and bile salts aid in the creation of colloidal structures such as unilamellar and multi- lamellar vesicles and mixed micelles, that further aid the solubilization of the drug substances.
It is for this reason that the vitro dispersion test should incorporate lipolytic components to render it more representative of in vivo conditions.
4. Determine the Optimal Filling Temperature
For SEDDS formulations to be effectively filled into capsules, the formulation filling temperature should be high enough to keep the formulation in a liquid state without affecting other aspects of the formulation. As part of the formulation development process, the optimal filling temperature should therefore be determined as well as the formulation’s viscosity at various temperatures and flow rates.
Useful Tips
Consider processing the formulations under vacuum
Manufacturing a SEDDS formulation can potentially introduce air into the formulation due to the necessity to mix different materials. Processing under vacuum can help prevent air from becoming incorporated into the product during mixing.
Use softgels in lieu of two-piece capsules for liquid SEDDS formulations
Softgels are more suitable for liquid formulations during large-scale manufacturing to remove the additional band-sealing step needed to prevent leakage observed with two-piece capsules.
Pay attention to small details
SEDDS formulations can be sensitive to variations in surfactant, aqueous phase and co-solvent levels. It is therefore important that lipid excipients are handled carefully in accordance with manufacturer-recommended instructions. A number of self-emulsifying excipients used in SEDDS are capable of absorbing moisture, therefore conditions of high humidity should be avoided.
Where semi-solid or solid excipients (such as Gelucire 44/14, Kollipho RH60, Dynasan 118 etc) are used it is advantageous to first gently melt them and homogenize the melt before sampling rather than scooping off material at the top.
Both the lipid and aqueous phases should be heated carefully to 50oC before mixing.
References
- Christopher Porter J H, et al: Enhancing intestinal drug solubilization using lipid-based delivery systems. Advanced Drug Delivery Reviews 2008; 60: 673–691.
- Christiansen ML, Holm R, Kristensen J, et al. (2014). Cinnarizine food-effects in beagle dogs can be avoided by administration in a self nanoemulsifying drug delivery system (SNEDDS).Eur J Pharm Sci 57:164–72
- Thomas N, Holm R, Müllertz A, Rades (2012). In vitro and in vivo performance of novel supersaturated self-nanoemulsifying drug delivery systems (super-SNEDDS). J Control Release 160:25–32




